
Getting Serious About Bariatric Surgery for Type 2 Diabetes
 Another new randomized, controlled study adds to the evidence that bariatric surgery for type 2 diabetes provides dramatically better control of the disease for people with obesity than intensive lifestyle therapy alone. Anita Courcoulas and colleagues from Pittsburgh have just published this study in JAMA Surgery.
Another new randomized, controlled study adds to the evidence that bariatric surgery for type 2 diabetes provides dramatically better control of the disease for people with obesity than intensive lifestyle therapy alone. Anita Courcoulas and colleagues from Pittsburgh have just published this study in JAMA Surgery.
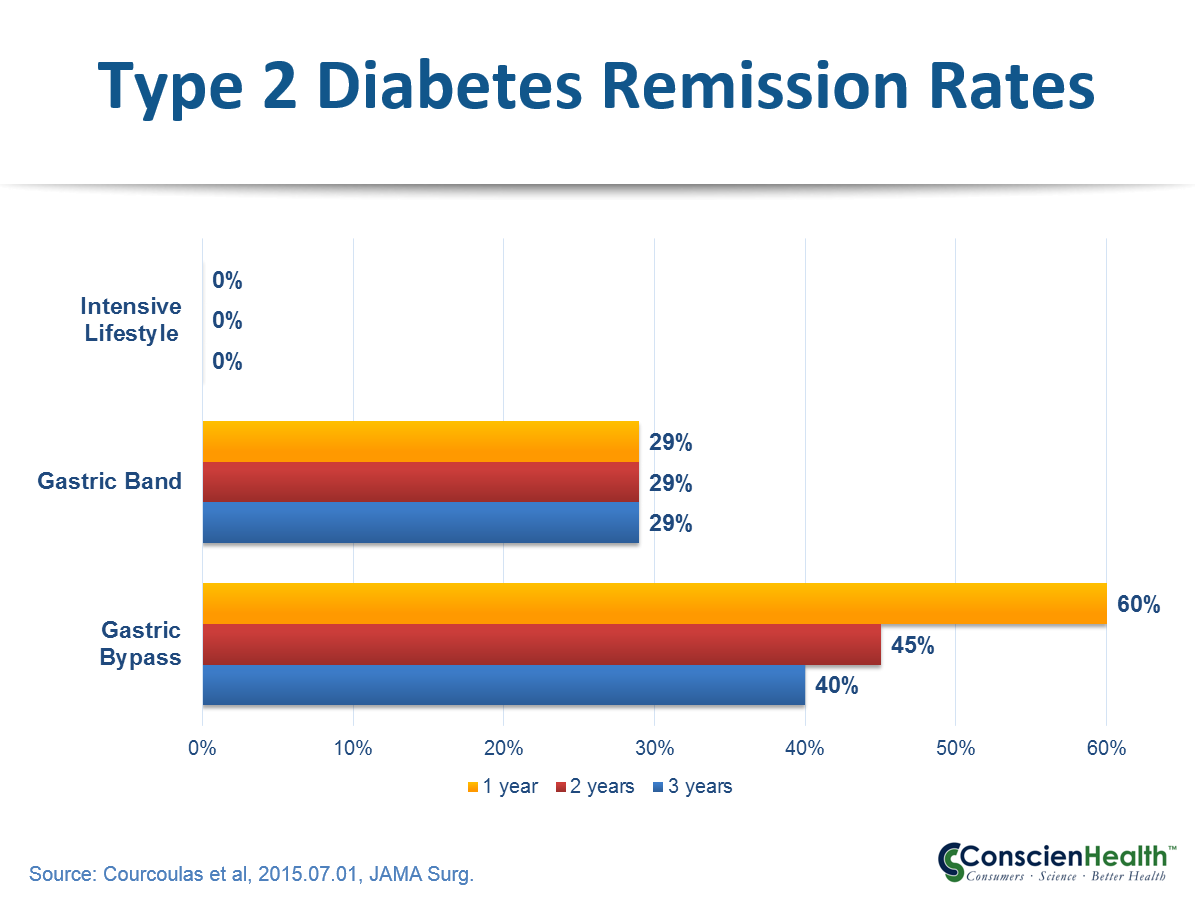
In this small, but well-controlled study, a total of 69 patients with obesity and type 2 diabetes were randomly assigned to receive either a year of intensive lifestyle weight loss therapy, a gastric band procedure, or a gastric bypass procedure. Nearly half (43%) of the patients had a BMI between 30 and 35.
At the end of three years, none of the people who received intensive lifestyle therapy had achieved remission of their diabetes, 29% of those in the gastric band group achieved remission, and 40% of the gastric bypass patients achieved remission.
In a companion editorial, Michel Gagner concludes:
We should consider the use of bariatric (metabolic) surgery in all severely obese patients with T2DM and start a mass treatment, similar to what was done with coronary artery bypass graft more than 50 years ago.
A year ago, the UK’s National Institute for Health and Care Excellence (NICE) recommended that all people with newly diagnosed type 2 diabetes and a BMI over 35 be offered early, rapid assessment for bariatric surgery.
Yet both clinicians and patients continue to drag their feet. People accept heart surgery for coronary disease much more readily than bariatric surgery for obesity and diabetes. Nobody really likes surgery and surgery for obesity just doesn’t feel as urgent.
What will it take, we wonder, to get serious about more intensive treatment for obesity, including bariatric surgery?
Click here to read more from Reuters, here to read the study, and here to read the editorial.
The Surgeon E. Pavlov in the Operating Theater, painting by Ilya Repin / WikiArt
Subscribe by email to follow the accumulating evidence and observations that shape our view of health, obesity, and policy.

July 07, 2015 at 8:30 am, Ellen Glovsky said:
This is all well and good. I wonder, however, what happened to those who did not “achieve” remission of DM2? And what about all of the malabsorption of nutrients caused by bariatric surgery? And what happens to all of those surgery patients further down the line? Do they stay in remission? Or have we cut up their GI tracts for nothing??
July 07, 2015 at 10:00 am, Ted said:
With or without bariatric surgery, people receive nutrition coaching in this study. And attention to good nutrition is important for post surgical patients. You choice of words — “we cut up their GI tracts” — is noteworthy.
Thanks for taking time to comment, Ellen.
July 07, 2015 at 10:49 am, Bruce Daggy said:
There is a challenge with the control group in a study like this. Presumably most everyone who volunteers for the study is hoping to get a free bypass. Randomized to the control group, obviously not a blinded outcome, they are disappointed. They may lack motivation to really engage with the lifestyle changes. It would be good to compare their zero percent success rate with what is seen in studies where the interventions were all non-surgical. It would be unfortunate if the take-away from this study was that lifestyle intervention is completely ineffective.
July 07, 2015 at 7:40 pm, Ted said:
You raise a good point Bruce. Thanks for bringing it up.
There is no attempt here to say that lifestyle intervention is ineffective — it’s a key part of surgical treatment. Lots of studies have shown how helpful intensive lifestyle interventions can be for improving the health of people with type 2 diabetes. In this study, they showed that people in the lifestyle group lost almost 6% of body weight and improved their lipid profiles and blood pressure.
However, it’s pretty clear that remission of type 2 diabetes is uncommon even with intensive lifestyle interventions. A study of intensive lifestyle intervention versus standard diabetes education found a remission rate (complete or partial) of 11.5% in a sample that included subjects with BMI>25. The complete remission rate was only 1.1%. You can find the study here: http://jama.jamanetwork.com/article.aspx?articleid=1486829
So yes, intensive lifestyle intervention is valuable, but it’s probably not a good bet by itself for effecting a remission of type 2 diabetes in people with obesity.
July 07, 2015 at 4:14 pm, BRENILDO M TAVARES said:
it is always very important every act against obesity the great problem of actual life
July 07, 2015 at 7:41 pm, Ted said:
Thanks for taking time to comment Brenildo. Certainly, obesity has a profound impact on quality of life and effective treatment significantly improves quality of life in people with obesity.
July 07, 2015 at 6:43 pm, Heather A. said:
What about quality of life for patients s/p gastric bypass? Really wondering what effect on their lives the surgery had for the 60% who did not “achieve remission.” And I’d love to ask everyone in the 40% who did achieve remission if they believe the surgery was worth it. Surgery, particularly surgery that alters absorption of nutrients, should be used only as a last resort.
July 07, 2015 at 8:12 pm, Ted said:
Heather, you are correct that quality of life is an important question. A considerable body of literature has been published on the impact of bariatric surgery on quality of life. Here is a link to a recent study in which you will find references to a lot of prior research on the subject: http://link.springer.com/article/10.1007/s11695-015-1717-4
The short and simple answer is that most people experience a substantial improvement in quality of life after bariatric surgery. That’s not to say that it’s a miraculous cure-all. Perhaps a quarter of patients (very rough estimate) have disappointing outcomes. Obesity is a very pernicious, persistent, and challenging chronic disease. You have better odds of being cured of many cancers than for being cured of obesity. Facing obesity is a long, hard slog and bariatric surgery is one of the best tools available.
July 08, 2015 at 12:08 pm, Heather A. said:
Thanks for the reference, Ted. In that study, I was disturbed to see that people with obesity who did NOT have obesity-related disease (problematic in and of itself, given that the conditions the researchers regard as obesity-related diseases also occur in people without obesity. Sure, the data show they occur more frequently in people with obesity, but obesity is not obligatory for any of these conditions mentioned) reported equal health-related quality of life as people with obesity who did have obesity-related diseases. Begs the question,why would that be? I suspect stigma from society at large, guilt, shame, and dissatisfying health care encounters play a large role in this. If so, why is surgery the answer, rather than something less invasive but with excellent health outcomes such as Health At Every Size? (I realize we’re talking about populations here. Of course, every person’s treatment approach should be individualized.)
Another point is that health-related quality of life is not the sum total of quality of life. It is absolutely a significant component of overall QoL, but we should take care not to conflate the two.
In participating in a HAES group, I’ve personally met more than 5 people who either themselves have died of complications from gastric bypass surgery or have a loved one who died of complications from gastric bypass surgery. I’m glad that you note it is not a cure-all. As someone with obesity, I am concerned that too great a focus on surgery for obesity conflates health with weight, interacts with societal weight stigma in problematic ways, and will begun to be pushed as a recommendation before other high quality, non-invasive interventions have been offered in good faith. In many cities, it’s easier to access bariatric surgery than a HAES group. We should ask ourselves why this is the case. I applaud the work you and your organization do to bring attention to the issue of access to health management for people with obesity. In addition to covering bariatric surgery for those individuals for whom it is truly the best option, all people with obesity should also have access to non-invasive evidence-based treatment approaches.
July 08, 2015 at 12:18 pm, Ted said:
Thanks for your thoughtful comments, Heather. Your comments about stigma, guilt, shame, and dissatisfying healthcare encounters are very important. It’s tough to make any progress in reducing the impact of obesity until we first treat people with respect regardless of their health and size.
July 08, 2015 at 8:00 pm, shelley kay said:
This is an impressive result in relation to the outcome of “diabetes remission”. In the context of health, exercise has effects on bone, muscle, fat, function, mood, cognition and inflammation. Myokines are secreted only when muscles contract. While surgery successfully reduces adiposity via energy restriction, it does not address the preservation of muscle and bone mass, both lost through surgery and inactivity. There may be individuals who have less regenerative potential in the beta cell due to factors other than the effects of excess adipose tissue. With all risk factors associated with diabetes, those who exercise have reduced mortality and morbidity. Lifestyle change takes longer to achieve modest but clinically significant outcomes. Both are important for different reasons in different time frames.
July 09, 2015 at 4:42 am, Ted said:
Thanks for taking time to comment, Shelley. You are correct that lifestyle changes are also helpful and important. In particular, physical activity has a big impact on bariatric surgery outcomes. It’s worth noting that surgery exerts its effects through more than just “energy restriction.” A great deal of research demonstrating that it acts to correct impaired signaling between the brain, gut, liver, pancreas, and adipose tissue. You can read more here: http://www.nature.com/nrgastro/journal/v10/n10/fig_tab/nrgastro.2013.119_F2.html
July 10, 2015 at 9:46 am, Bruce Daggy said:
Thanks for the reference, Ted. The surgical study also defined success as partial or complete remission, so the intensive lifestyle intervention (ILI) study supports my point that the zero percent finding in the surgical study likely due to either the desire for surgery among those randomized to the control group, or the control intervention being sub-optimal. I’m not opposed to bariatric surgery, but if out of every 100 people who would elect surgery for weight loss and diabetes management, about 10 could use ILI to lose weight and get off all meds, and a larger number could lose weight and get off some drugs, it seems to me that we’re not making the best use of ILI. We’re also not doing enough to intervene at the pre-diabetes stage, but that’s another topic.
July 10, 2015 at 11:30 am, Ted said:
Thanks, Bruce, for following up. No doubt you know the importance of taking care when comparing across studies in different patient populations. The ILI study included people down to a BMI of 25 while the surgery study was only people who actually had obesity. So the comparisons remain tricky.
Not withstanding that caution, I agree that we need to make good use of all the tools we can. My doctor doesn’t care about my weight. (“It’s not a problem,” he told me dismissively on my last visit.) He just seems eager to see my lipids and hypertension progress to a level where he can prescribe some drugs.