
A Double Dose of Discrimination
A pair of presentations at the 31st Harvard Blackburn Course in Obesity Medicine reminds us of much work to do. We have an embarrassing gap in respectful and equitable care for people with obesity. Scott Kahan gave a compelling overview of weight bias and stigma. On top of that, Fatima Cody Stanford described the added heath burden of obesity that comes with racial and ethnic minority status. It’s a double dose of discrimination.
Respect
 Perhaps the most jolting observation is blatant disrespect. Kahan explained how persons living with obesity will routinely encounter disrespect from healthcare providers. And he offered objective data to show just how stark this problem is.
Perhaps the most jolting observation is blatant disrespect. Kahan explained how persons living with obesity will routinely encounter disrespect from healthcare providers. And he offered objective data to show just how stark this problem is.
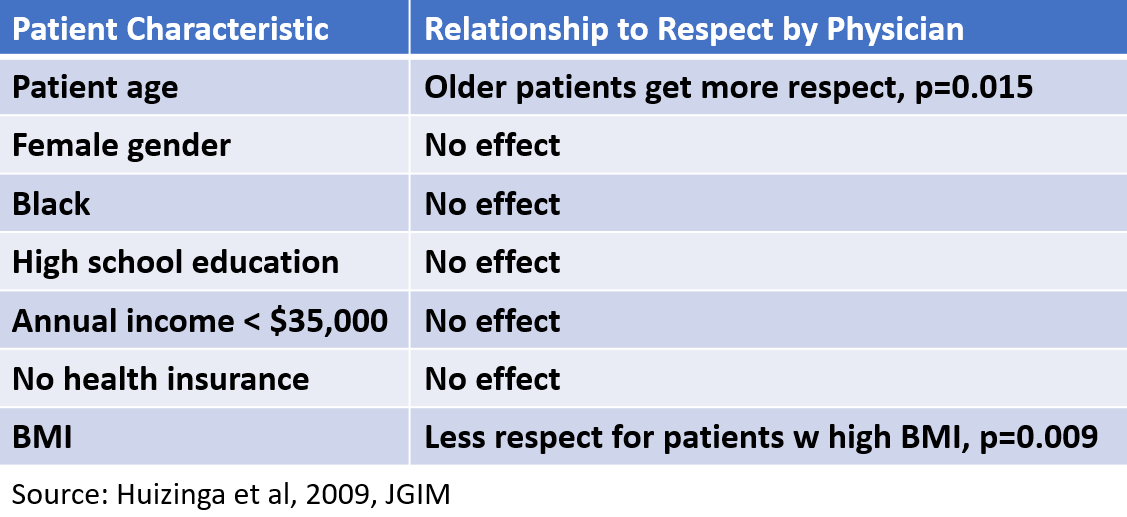
Generally, physicians regard all kinds of patients with respect. In a study by Mary Margaret Huizinga and colleagues, this was rather clear. Gender, race, education, income, and health insurance seemed to make no difference. Physicians were no more or less likely to respect patients based on these factors. However, they did express a bit more respect for older patients. We get it. Respect your elders.
Unfortunately, a patient’s size makes a significant difference. In fact, it was the biggest factor in how much physicians respected different patients. Physicians were clearly more likely to express low respect for patients with a high BMI.
Now, let’s remember respect is a core concept for practicing medicine. It’s tough to be a good doctor without respecting patients. Moreover, the quality of care suffers without respect. Health suffers, too. Patients avoid disrespectful providers. It’s a vicious cycle.
Racial and Ethnic Disparities Compound the Harm
Stanford explained that racial and ethnic disparities magnify these problems. The risks for obesity are higher for many racial and ethnic minorities. Social and economic factors can amplify that risk. U.S. born black women have twice the risk of obesity as white women.
And yet, doctors are less likely to diagnose the disease in black women. Furthermore, average treatment outcomes are not as good. So many questions remain. Why is the impact greater for ethnic and racial minorities? How can we erase the disparities in diagnosis and treatment?
Stanford left us with a hopeful message from a series of case histories. With skillful use of evidence-based tools, good outcomes are possible. We can set aside ethnic and minority status in the clinic. It all starts with a diagnosis and respectful medical care.
Click here for the study by Huizinga et al and here for Stanford’s slides.
Seriously? photograph © Obesity Action Coalition / OAC Image Gallery
Subscribe by email to follow the accumulating evidence and observations that shape our view of health, obesity, and policy.
Month x, 2018
