
Less Beef = Less Carbon and More Health?
 The NRDC has a little ray of sunshine for us this week. Americans are eating less beef and that means less carbon going into the atmosphere to heat up the planet. It might also mean healthier dietary patterns.
The NRDC has a little ray of sunshine for us this week. Americans are eating less beef and that means less carbon going into the atmosphere to heat up the planet. It might also mean healthier dietary patterns.
The Environmental Impact of Beef Production
Meat production creates a lot of greenhouse gases. And beef is an especially important source. NRDC estimates that beef is responsible for 34% of the greenhouse gas from producing food for Americans. Why? Well for starters, cows are little gas machines. The methane in their burps and farts is far more potent than carbon dioxide for warming the planet. The average cow produces enough methane in a year to heat up the planet as much as four tons of carbon dioxide would.
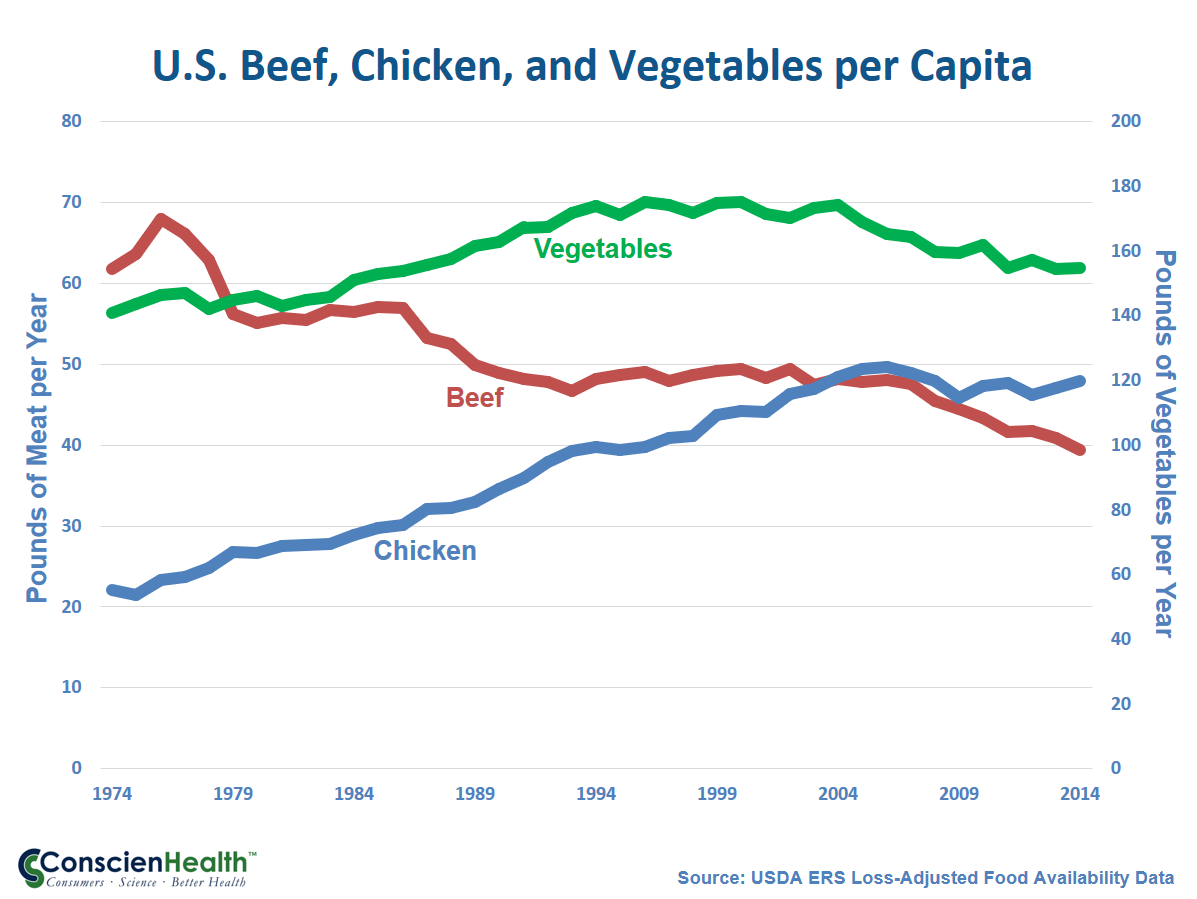
So the steady drop in the American appetite for red meat has driven a drop in greenhouse emissions. In fact, greenhouse gases attributable to our food have come down by 10% over the last decade.
A Health Benefit?
When USDA and HHS released the 2015 Dietary Guidelines for Americans, recommendations on red meat were a big bone of contention. The Scientific Report of the Guidelines Advisory Committee had come down hard on red meat. The final guidelines danced around the subject. Instead of advising people to eat less red meat, they advised eating more of other types of protein.
Nutrition experts are pretty confident that the saturated fat in red meat is a problem for heart disease in the American population. But it matters what people substitute when they eat cut down on saturated fats. We learned the hard way that replacing saturated fats with carbs is not a good tradeoff. And that’s how we got the advice to eat more of other sources of protein.
Advice to “eat more” always goes over with food lobbyists better than advice to “eat less.”
Regardless of this little tap dance, you can see in the graph above that consumers seem to be getting the message about red meat. The decline continues. So Americans may well benefit from consuming less red meat and saturated fat. And your planet thanks you, too.
For the report from NRDC, click here. For perspective from Mashable, click here.
Cows in Field, photograph © Frank DiBona / flickr
Subscribe by email to follow the accumulating evidence and observations that shape our view of health, obesity, and policy.
March 25, 2017

March 25, 2017 at 11:19 am, David Brown said:
“Nutrition experts are pretty confident that the saturated fat in red meat is a problem for heart disease in the American population.”
It’s interesting that T. Colin Campbell, who is against meat consumption of any sort, blames the protein, not the fat. In 2014 he wrote, “I propose that this argument for or against saturated fat should have been moot from the very beginning of this research. Here’s why. The original hypothesis that dietary fat, especially saturated fat, is chiefly responsible for heart disease began with laboratory studies over a century ago[10] and the findings ere, at best, uncertain. Much more impressive evidence also was published to show that the early stages of heart disease, atherosclerosis, and its predictive serum cholesterol marker, were increased much more by dietary protein than by dietary fat, especially the protein in animal-based foods.” http://nutritionstudies.org/fallacious-faulty-foolish-discussion-about-saturated-fat/
In 2015 he wrote, “This latest 2015 DG report repeatedly assumes that saturated fat is independently unhealthy, thus recommending that its intake be controlled. This interpretation is short-sighted because it tends to suggest that unsaturated fats should be preferred. In contrast, about 30-40 years ago, in experimental animal studies on mammary cancer unsaturated fats were shown to promote cancer substantially more than saturated fats…” http://nutritionstudies.org/2015-dietary-guidelines-commentary/
In 2016 he wrote, “Then, there’s another twist that is very important to consider. Unsaturated fat (PUFAs) are susceptible to tissue damaging oxidation, and saturated fat is not. Oxidation brings into consideration the formation of chemically reactive oxygen (as ‘reactive oxygen species, ROS) that causes aging and increases cardiovascular disease and cancer. For example, plant oils experimentally promote cancer much more than does saturated fats—that’s right. This is an experimental observation that is at least 30-40 years old.” http://nutritionstudies.org/plant-oils-are-not-a-healthy-alternative-to-saturated-fat/
Campbell may be on to something. High animal protein intake does appear to be problematic for health. But not because of the protein. More likely it is the arachidonic acid content in cell membranes that are the root cause of inflammation. Animal feed rich in linoleic acid boosts the arachidonic acid content of cell membranes. Here’s how that works.
Traditionally, animals grazed. Grass contains ALA (ω-3), whereas grains, corn and soya (which are now fed to animals) are high in LA (ω-6). This imbalance in the amount of ω-6 and ω-3 fatty acids is a new phenomenon that was never a part of human evolution. Human beings evolved on a diet that had equal amounts of ω-6 and ω-3 fatty acids. This balanced ratio of ω-6 to ω-3 is critical to human development during pregnancy and lactation, in the prevention of chronic diseases and in their management. The typical Western diet now provides an ω-6 to ω-3 ratio of around. High dietary intake of ω-6 fatty acids as occurs today leads to increases in white adipose tissue and chronic inflammation, which are the ‘hallmarks of obesity’. http://openheart.bmj.com/content/3/2/e000385
Arachidonic acid (AA) in the diet can be efficiently absorbed and incorporated into tissue membranes, resulting in an increased production of thromboxane A2 by platelets and increased ex vivo platelet aggregability. Results from previous studies have shown that AA is concentrated in the membrane phospholipids of lean meats. http://bmcresnotes.biomedcentral.com/articles/10.1186/1756-0500-5-97
The highest level of AA in lean meat was in duck (99 mg/100 g), whereas pork fat had the highest concentration for the visible fats (180 mg/100 g). The lean portions of beef and lamb contained the higher levels of n-3 polyunsaturated fatty acids (PUFA) compared with white meats which were high in AA and low in n-3 PUFA. The present data indicate that the visible meat fat can make a contribution to dietary intake of AA, particularly for consumers with high intakes of fat from pork or poultry meat. https://www.ncbi.nlm.nih.gov/pubmed/9590632
The experts who believe saturated fat intake is linked to heart disease also promote the idea the high linoleic acid intake, because it lowers cholesterol, protects arteries from clogging. However, “Linoleic acid has been found to modulate endocannabinoid synthesis due to its ability to be converted to AA by the human body, although the effect of dietary linoleic acid on human endocannabinoid synthesis has not been investigated.” https://www.hindawi.com/journals/ije/2013/361895/
That was 2013. In 2016 this comment was published. “While everyone consumed the same amount of plant oil (LA), the insertion carriers accumulated far higher blood levels of the omega-6 arachidonic acid (ARA), which is proinflammatory. Unfortunately, they also made much less anti-inflammatory omega-3 acids – EPA and DHA because their conversion machinery was overwhelmed with producing ARA. This imbalance in omega-6 and omega-3 LCPUFA can have serious health implications. “Of course, Omega-6 is an essential nutrient, but it’s too much of a good thing. That we need to worry about,” Brenna cautioned. http://www.biotechniques.com/news/Do-Vegetarians-Have-Better-Metabolisms/biotechniques-364804.html#.WNaIkPkrK72
Note that Brenna was a member of the 2015 Dietary Guidelines Advisory Committee and the only member besides Gary Foster (who resigned) who seems to be familiar with endocannabinoid system research.