
The Collapse of Trust in Top-Down Public Health
Two years ago, 69 percent of Americans believed what the CDC had to say. Now, that number is 44 percent. After seven decades, CDC sat atop a pyramid of influence in public health. But today, top-down public health decrees meet with skepticism as often as with trust. We are living in an era when distrust is now the default, says Edelman in their latest Trust Barometer report.
Certainly, in obesity-related public health policy, decrees of this is what’s good for you have failed to bring change. Maybe, just maybe, it’s time for a bottom up orientation that respects the lived experiences of people with obesity and overweight.
Lessons from Colonial Public Health
Our friend Philippa Sandall recently pointed us to a history of efforts to control bubonic plague. In the colonial empire of Great Britain, top down strategies were not working too well at the turn of the twentieth century. So a medical service officer, Andrew Buchanan, learned from the success of a tiny village in western India that consistently avoided ravages of plague. It was due to their large population of cats.
Buchanan became an advocate of bottom up public health strategies that defied colonial norms and drew upon grass-roots wisdom. Cats became an animal technology for controlling the plague. Projit Bihari Mukharji describes the implications:
“Unlike Buchanan’s efforts to learn from colonised communities and their practices, public health views ‘from below’ usually remained distinct and separate from the vertically organised public health campaigns – especially in the colonies. What stands out most about Buchanan’s scheme is his own, explicit insistence that his scheme was a ‘People’s Remedy.’ In giving credit, finding data, and actively seeking to align the scheme with local cultural mores, Buchanan tried hard to live up to the moniker of a ‘People’s Remedy.’ This was rare in histories of public health in general and colonial public health in particular.”
Discounting the Affected People
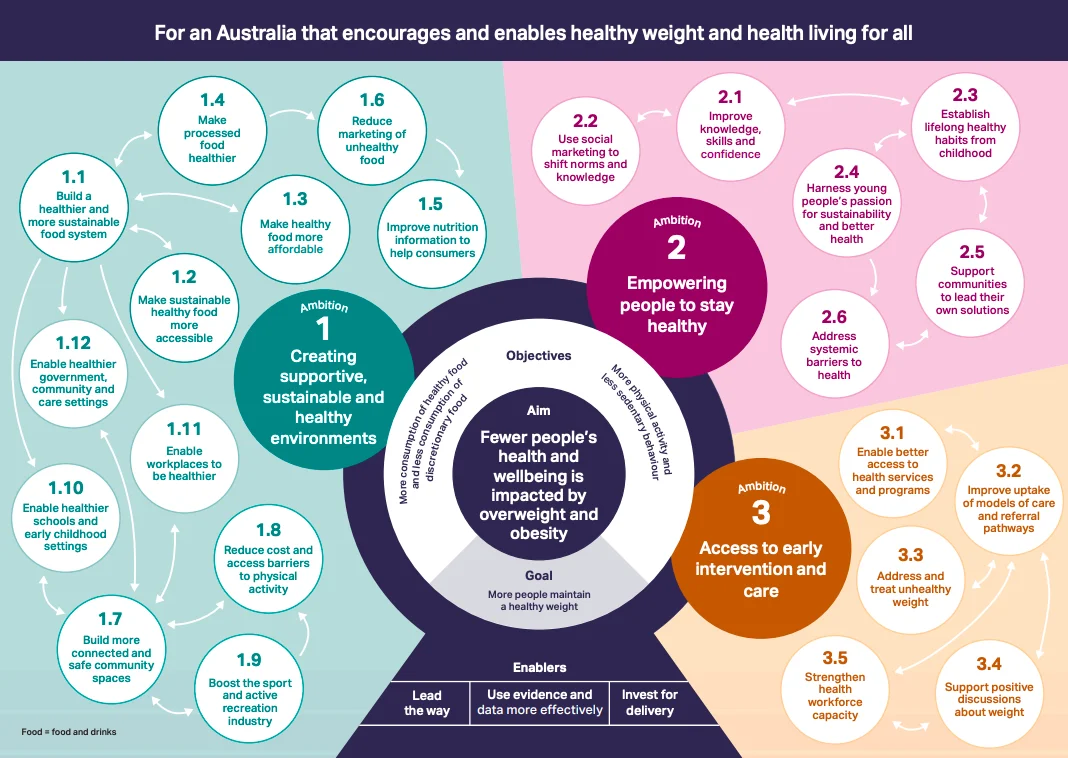 Because of entrenched, implicit bias, the impulse is to dismiss the people who are living with obesity in public health strategies to address it. For example, in the new National Obesity Strategy for Australia, lived experiences of people with obesity are an afterthought. A quick look at their schema reveals a strong emphasis on educating and nudging people to “stay healthy.”
Because of entrenched, implicit bias, the impulse is to dismiss the people who are living with obesity in public health strategies to address it. For example, in the new National Obesity Strategy for Australia, lived experiences of people with obesity are an afterthought. A quick look at their schema reveals a strong emphasis on educating and nudging people to “stay healthy.”
But VicHealth CEO Sandro Demaio correctly says that “relying on behaviour change is simply not going to move the needle.”
Nevertheless, that is the default thinking in most public health strategies for obesity. This is what’s good for you and you are going to have to change your ways.
More than a century ago, Buchanan found a better way. Get curious about the experiences of real people. Build your strategies from the bottom up. It’s an excellent way to foster trust and find an effective path forward.
Click here for Mukharji’s account of Buchanan’s efforts to learn from real people. For more about the Australian obesity strategy, click here.
Colonial Policy, painting by Pavel Filonov / WikiArt
Subscribe by email to follow the accumulating evidence and observations that shape our view of health, obesity, and policy.
April 10, 2022

April 10, 2022 at 8:54 am, Allen Browne said:
Interesting but:
The basic problem is that we don’t know what disturbs a healthy ERS and makes it go awry
1. Ambition #1 – Supportive, sustainable, and healthy environments have not been shown to change the rate of the development of obesity or to lessen the incidence of obesity. I.e. we don’t know what causes one person to develop obesity and another to not develop obesity.
2. Ambition #2 – See #1. This puts the responsibility on the patient and not on the health care system. I.e. – If they are not healthy, it is their fault.
3. Ambition #3 – Good idea. Has to be done without blame and fault finding. Has to be done with education about obesity as a disease.
My thoughts are nothing original – just looking at the data we currently have..
Oh well🥲.
Allen
April 10, 2022 at 9:07 am, David Brown said:
I like this post. In my view, the reason CDC strategies for protecting and improving the public health don’t work is because they are guided, at least in part, by myth. As John F. Kennedy noted in his June 11 1962 Commencement Address at Yale University, “The great enemy of truth is very often not the lie–deliberate, contrived and dishonest–but the myth–persistent, persuasive and unrealistic. Too often we hold fast to the cliches of our forebears. We subject all facts to a prefabricated set of interpretations. We enjoy the comfort of opinion without the discomfort of thought.”
For anyone curious as to what sort of myth shapes public health policy, I suggest you watch some of these videos. https://www.youtube.com/playlist?app=desktop&list=PLpAsu_3KtxQN21LYCu6NyqYGthtlYL5cG