
Hammering Away at Diets to Reverse Obesity
“Especially for children, diet and lifestyle must remain at the forefront of obesity prevention and treatment.” This conviction, summing up a new editorial in JAMA, beautifully captures the discomfort that the availability of more effective treatments for obesity causes. The belief persists that diets and exercise are the right way to reverse obesity. So the gut reaction to other options is to regard them as a threat to the order of things.
A Jumble of Arguments
Though their bottom line is clear enough, David Ludwig and Jens Holst present quite a confusing jumble of arguments to take us there. They falsely assert that guidance from the American Academy of Pediatrics for treating obesity “emphasizes weight loss drugs and bariatric surgery.” We have to wonder if they are relying on sensational editorials for their understanding of those guidelines.
In fact, the AAP guidance is quite clear that obesity is a complex, chronic condition. It doesn’t have a simple fix. Dietary and behavioral support is essential, says the guidance:
“The foundation of all comprehensive obesity treatment is helping the child/adolescent and the family change lifestyle, behavioral, and environmental factors that will allow them to manage their obesity in their individual health and environmental context.”
Starting with the premise that they are defending against an excessive reliance on drugs and surgery, Ludwig and Holst present arguments about the value of low-glycemic diets, paltry funding for nutrition research, the need to test novel diets, and the importance of social justice. At the end of this buffet line of rationales, their conclusion is quite clear. Changing diets and lifestyles must be the right way to reverse obesity trends.
More Than Nutrition
 The core problem with the argument is that obesity is not solely a dietary problem. Aaron Kelly, co-director of the Center for Pediatric Obesity Medicine at the University of Minnesota, points out that we actually have a lot of research on dietary approaches for childhood obesity and the benefits have been modest at best:
The core problem with the argument is that obesity is not solely a dietary problem. Aaron Kelly, co-director of the Center for Pediatric Obesity Medicine at the University of Minnesota, points out that we actually have a lot of research on dietary approaches for childhood obesity and the benefits have been modest at best:
“Let’s break the cycle of doing the same things repeatedly and expecting different results. Most pediatric obesity studies are behavior and diet-related. It’s no coincidence that the contemporary focus targeting biology (a root cause) with medicine produces superior results.”
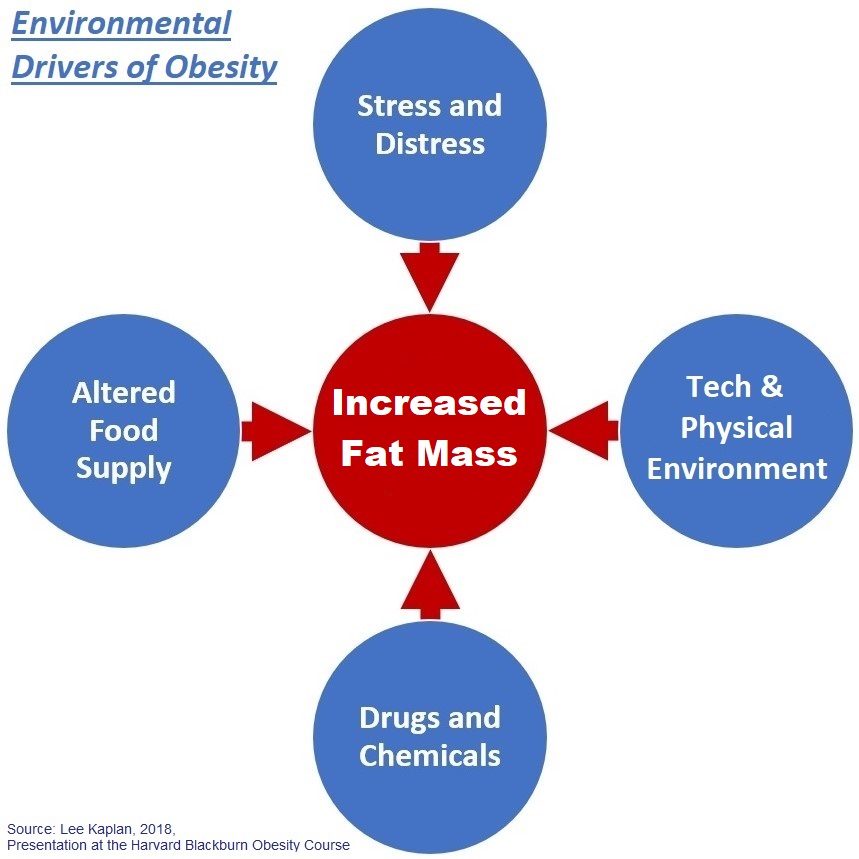
The fact is that obesity is a complex chronic disease that results from the interaction of human physiology with environmental factors that promote it. Those factors have risen to create the increases we see in obesity prevalence. They involve much more than just nutrition and the food supply.
Focusing exclusively on food as the cause of obesity for decades has only brought us failure in efforts to reverse the trends. If we continue hammering away mainly on diets and nutrition to overcome obesity, we will doom ourselves to continued failure.
A more complete and systematic approach is necessary. Nutrition is an important part, but not the whole of it.
Click here for the editorial by Ludwig and Holst, here for more on the causes of obesity.
Subscribe by email to follow the accumulating evidence and observations that shape our view of health, obesity, and policy.
May 2, 2023

May 02, 2023 at 7:49 am, Allen Browne said:
Yup!
I couldn’t have said it better myself. Obesity is a complex, heterogenous chronic disease that destroys lives.
Allen
May 02, 2023 at 1:31 pm, Jim Hershey said:
I struggle when I hear lifestyle interventions and “diet and exercise” are the only interventions mentioned. Especially with adolescents, sleep dysregulation and the chronic stress state of kids that struggle with obesity (or any teen nowadays) have to be considered as prime movers in treating obesity. We are too well aware of the sympathetic response and what it does in regards to energy craving and storage to continue to leave it out of the conversation, especially when it’s included in a four “environmental driver” diagram.
For the last 4 years Gem Academy has been averaging 38% loss over 12 months with adolescent girls with lifestyle intervention alone. With a (mostly) whole food, ad libitum diet, no rigorous activity AND regulated sleep cycle & duration along with an extensive therapeutic and mindfulness program.
This approach is out performing medication and surgery and where a residential program is not scalable for the masses the lessons and evidence certainly need to be taken into consideration.